Dermatophytosis, a fungal infection of keratinized tissues, remains a common clinical entity in veterinary medicine. Its polymorphic presentation, coupled with the diversity of etiological agents and the inherent limitations of each diagnostic tool, can sometimes transform its identification into a real challenge.
During the last NAVDF congress held in Orlando last April, Professor Ross Bond from the Royal Veterinary College in London conducted an in-depth analysis of the epidemiological, clinical, and diagnostic aspects of dermatophytosis, highlighting pitfalls to avoid and offering perspectives for an informed approach, essential for optimal management.
1. Introduction: The Inherent Complexity of Dermatophytes
Dermatophytosis, although familiar to practitioners, hides a complexity that deserves sustained attention. Caused by keratinophilic fungi, mainly from the Arthrodermataceae family, this condition affects hair, claws, and the stratum corneum [1]. While the genera Microsporum and Trichophyton are historically the most incriminated in animals, fungal taxonomy is constantly evolving. The advent of molecular mycology has revealed new genera, such as Nannizzia and Arthroderma, which might be mentioned more frequently on laboratory reports [2]. Epidermophyton, on the other hand, remains rare in animal pathology, its tropism being almost exclusively human. Faced with this etiological diversity and a kaleidoscope of clinical manifestations, how can veterinarians navigate with confidence towards an accurate diagnosis?
2. Epidemiology and Spectrum of Dermatophytes
Understanding the ecology and distribution of dermatophytes is a crucial first step to comprehending their pathogenicity.
2.1. Ecological Classification: A Fundamental Triad
The traditional ecological classification distinguishes three main categories of dermatophytes, knowledge of which guides clinical suspicion and the search for the source of infection:
-
Zoophilic: These species, such as the paradigmatic Microsporum canis (mainly in cats), are adapted to animals and are easily transmitted between them. Their identification often involves investigation of the environment and congeners.
-
Geophilic: These fungi, of which Microsporum gypseum is a typical representative, find their reservoir in soil where they degrade keratin. Contact with contaminated soil is therefore the main mode of transmission.
-
Anthropophilic: Specifically adapted to the human host, these dermatophytes, such as Trichophyton rubrum, are less frequently the cause of reverse zoonoses (from human to animal) but this possibility should not be ruled out.
2.2. Geographic Distribution and Host Specificity: Variations to Consider
The prevalence of different dermatophyte species is not uniform, varying significantly by geographic region and animal species concerned.
-
In cats, Microsporum canis reigns supreme worldwide [3].
-
In cattle, Trichophyton verrucosum is the major etiological agent of ringworm, with an equally global distribution.
-
In equines, Trichophyton equinum is frequently isolated, but it is interesting to note the existence of strain variations, such as the distinct one identified in Australia [4].
2.2.1. The Case of Dogs: A Nuanced Epidemiological Picture
The epidemiology of canine dermatophytosis particularly well illustrates this geographical variability:
-
In the United Kingdom, long-term studies, particularly a 35-year survey in Bristol analyzing 475 isolates, have highlighted the predominance of M. canis (about two-thirds of cases) followed by Trichophyton mentagrophytes (about a quarter) [5]. A more recent follow-up study over 26 years in the same region confirmed this trend, with figures of 42% for M. canis and 38% for T. mentagrophytes [6].
-
In the United States, a 1991 study conducted at Louisiana State University reported 43% M. canis and 11% T. mentagrophytes [7]. An older CDC survey from 1958, involving 368 isolates from 35 states, showed a proportion of 69% for M. canis and 11% for T. mentagrophytes [8].
It appears, therefore, that T. mentagrophytes plays a proportionally more important role in dogs in the UK than in the US, even though M. canis remains a key pathogen in both regions. What environmental or host-related factors could explain these differences?
2.2.2. Other Notable Dermatophytes and Their Ecological Reservoirs
Vigilance is also necessary for other less frequent species whose identification may have clinical and epidemiological implications:
-
Trichophyton erinacei: This agent, responsible for “hedgehog ringworm,” sees its prevalence directly correlated with the presence of these insectivores.
-
Trichophyton verrucosum: Mainly transmitted by cattle, it is rarely diagnosed in dogs in the United States, and only sporadically in the United Kingdom.
-
Microsporum persicolor: With voles and mice as its main reservoir, this dermatophyte is uncommon in dogs in the UK and has not been reported in this species in the US, although its presence in North America (e.g., Ontario, Canada) is confirmed [9].
-
Microsporum gypseum: This geophilic fungus is a major causative agent of dermatophytosis in Louisiana (44% of canine cases) and remains significant in other American studies (18% of cases). In stark contrast, in Bristol, it took 35 years to isolate M. gypseum from only four dogs. This disparity raises the question of the influence of pedoclimatic factors, with warmer soil in the United States possibly favoring its survival and proliferation.
2.3. Predisposing Factors: Identifying Subjects at Risk
Certain factors intrinsic to the animal or related to its environment can increase its susceptibility to dermatophytosis:
-
Age: Young animals, with still immature immune systems, are classically considered more vulnerable to infection by M. canis. Conversely, older animals, if they are better hunters, might be more exposed to dermatophytes transmitted by wildlife.
-
Breed: Breed predispositions have been suggested. Yorkshire Terriers seem more susceptible to M. canis (in the UK), while Jack Russell Terriers might be more prone to dermatophytoses acquired from wildlife. Long-haired cats, such as Persians, are also frequently cited.
-
Seasonality: While few marked seasonal variations are noted in the UK, an American study suggested an increased incidence of T. mentagrophytes in autumn.
3. The Polymorphic Face of Dermatophytosis: Recognizing the Signs
Dermatophytosis is a “great imitator.” Its clinical presentation can be so varied that it requires the practitioner to maintain a high index of suspicion. As Michael Schaer reminded, “If you don’t think about it, you won’t find it” [10] – an adage particularly relevant here.
3.1. Classic Presentations: The Warning Signs
Some manifestations are considered more typical, though not pathognomonic:
-
In cattle (T. verrucosum): Characteristic lesions, well-circumscribed, alopecic, covered with thick grayish scales, preferentially located on the head, neck, and ears. These lesions are more frequent in animals confined indoors during winter.
-
In dogs and cats (M. canis): The classic lesion is a circular, scaly, sometimes erythematous and crusty alopecia, often located on the head. However, less inflammatory forms, limited to an area of alopecia without marked cutaneous reaction, are also observed.
It’s always important to keep in mind Danny Scott’s warning: “If it looks like ringworm [in dogs], it probably isn’t. It’s probably staphylococcal folliculitis.” [11]. Indeed, in dogs, expanding annular lesions are more often of bacterial origin.
3.2. Atypical Forms and Diagnostic Pitfalls
This is where diagnosis can become a real exercise in subtlety:
-
Folliculitis and Furunculosis of the Muzzle (Sylvatic Dermatophytes): Frequently associated with T. mentagrophytes or T. erinacei in dogs with contact with rodents or hedgehogs (hunting dogs, terriers). These lesions can be unilateral or asymmetric, with a tendency toward central healing and active peripheral inflammation. The planum nasale is typically spared.
-
Nodular Lesions and Plaques (Kerion, Pseudomycetoma):
-
A Jack Russell Terrier that explored a rabbit burrow developed an erythematous, squamo-crusted plaque on the chest, as well as a distinct nodular lesion on the carpus, both confirmed to be due to T. mentagrophytes.
-
A Doberman presenting with multiple erythematous plaques, initially suspected of cutaneous lymphoma, was found to have dermatophytosis due to T. mentagrophytes. What a surprise for the clinician facing this unexpected diagnosis!
-
In Persian cats, pseudomycetoma (or deep kerion) caused by M. canis is a well-described entity, manifesting as nodules, fistulous tracts, and sometimes the expulsion of grains reminiscent of “sulfur grains.”
-
A case reported in Croatia describes a kerion in a cat – a fluctuant and purulent nodule – caused by M. gypseum in association with staphylococcal superinfection.
-
-
Irregular and Subtle Lesions: A hunter cat presented with discrete alopecia on the muzzle and erythemato-squamous lesions on the pinna due to T. mentagrophytes, a species yet uncommon in felines. This underscores the importance of not relying solely on classic fungal species/host associations.
-
Nosocomial Infections: Dermatophytosis lesions can develop at sites previously clipped for surgery or intravenous catheter insertion. Rigorous hygiene of clipping equipment, with systematic disinfection between each animal, is therefore a significant preventive measure.
-
Generalized Scaly Form (M. persicolor): Unlike most other dermatophytes, M. persicolor does not invade the hair shaft but colonizes only the stratum corneum. This results in generalized scaling, sometimes intense, without significant alopecia. An illustrative case is that of a dog with a four-year history of generalized scales, finally diagnosed as an infection with M. persicolor.

Very extensive form of feline dermatophytosis
3.3. Special Cases: Guinea Pigs and Rabbits – The Trap of Asymptomatic Carriage
These small mammals, particularly those from pet shops or collections, can be asymptomatic carriers of the T. mentagrophytes complex (frequently identified by molecular techniques as T. benhamiae). This asymptomatic carriage represents a major challenge for infection control.
-
Prevalence of asymptomatic carriage:
-
In Belgian pet shops, studies have shown that 3.5% of guinea pigs and 3.8% of clinically healthy rabbits were carriers [12].
-
In Slovak pet shops, these figures rose to 10% for guinea pigs and 6% for healthy rabbits [13].
-
A study conducted in Berlin pet shops, using PCR, revealed that while 9% of guinea pigs had clinical lesions, a staggering 90% of all guinea pigs tested were carriers of T. benhamiae DNA [14]. These figures are concerning regarding the potential source of infection for other animals or humans.
-
-
Clinical cases (rabbits in Spain): Among rabbits with clinical lesions of dermatophytosis, 54% of isolates corresponded to T. mentagrophytes and 27% to M. canis [15].
3.4. Dermatophytosis as a Zoonosis: A Constant Concern
It is imperative to remember the zoonotic potential of dermatophytosis. Numerous cases of transmission to humans are documented, affecting both owners (and their children, as illustrated by a case of transmission from an infected guinea pig) and veterinary staff (a neurology resident who contracted the infection from a canine patient).

Human contamination by a dermatophyte
4. Diagnostic Strategies: Towards a Multimodal Approach
The diagnosis of dermatophytosis does not rely on a single infallible test. A multimodal approach, combining clinical examination with various complementary tests, is key.
4.1. Direct Microscopic Examination (Trichogram): The First Examination to Perform
This simple and quick examination can provide valuable clues.
-
Technique: Hair should be collected from the active periphery of lesions, targeting those that appear “cottony,” broken, or abnormal. The sample is mounted between a slide and coverslip, classically in a drop of 10-20% KOH (which helps clarify keratinic debris) or simply in mineral oil. The crucial step is to lower the microscope condenser and manipulate the diaphragm to increase contrast, as fungal elements are often not very refringent in white light. One looks for the presence of ectothrix arthrospores (forming a sheath around the hair) or endothrix segmented hyphae (inside the hair shaft).
-
Sensitivity: The Bristol study, comparing microscopy to culture, reported an overall sensitivity of 55%. It was higher for M. canis (58%), often associated with abundant easily visible spore production, than for T. mentagrophytes (44%), where hyphae may be more discrete and located in scales. The sensitivity is likely lower for less experienced practitioners.
-
Pitfalls and artifacts: Confusion is possible with artifacts such as inner or outer hair sheaths, keratin debris, air bubbles, or saprophytic fungal conidia that can contaminate the skin surface. A good knowledge of fungal morphology is essential.
-
Adjuvant stains: Although not essential if the lighting technique is mastered, stains such as “Potash Kwik” (a commercial KOH solution containing ink) or Parker ink can help to contrast fungal elements. Calcofluor White is a more sophisticated option (see section 4.5).
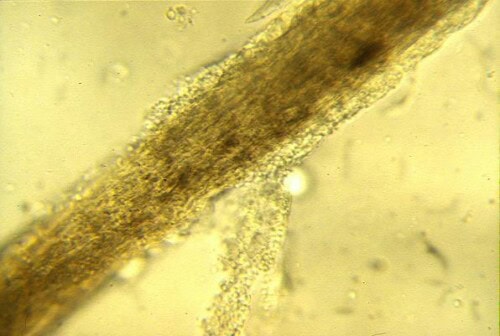
Ringworm-infected hair
4.2. Wood’s Lamp: A Classic Tool with Known Limitations
The Wood’s lamp remains a useful tool, provided its specificities are known.
-
Principle and fluorescence: Some strains of M. canis (but not all) produce, during their metabolism, pteridine, a substance that emits a characteristic apple-green fluorescence when exposed to ultraviolet light of a specific wavelength (around 365 nm). It is important to note that it is the actively infected hairs that fluoresce, not scales, crusts, or colonies in culture.
-
Specificity and limitations: This examination is primarily relevant for suspected infection with M. canis. The majority of Trichophyton species do not produce this fluorescence. Moreover, even for M. canis, not all strains are fluorescent.
-
Optimal examination conditions: To maximize detection chances, the examination must imperatively be performed in a completely dark room. The lamp must be properly preheated for several minutes before use. The use of a quality Wood’s lamp, specifically designed for veterinary use and ideally equipped with a magnifying lens, is strongly recommended.
-
Sensitivity: For M. canis infections, the sensitivity of the Wood’s lamp varies according to studies, generally ranging between 54% and 70% [16]. A negative result, therefore, never excludes dermatophytosis.
4.3. Fungal Culture: Identification and Viability
Fungal culture remains a reference method for precise species identification and confirmation of pathogen viability.
-
Sample collection: Hair and scales or crusts should be taken from the periphery of the most active lesions. For screening asymptomatic carriers or monitoring therapeutic efficacy, the sterile brush method (McKenzie brush type) passed over the entire coat, or the use of agar plates with a textured side for sampling (like Derm-Duet), are proven techniques.
-
Culture media: Sabouraud Dextrose Agar (SDA) is the classic base medium commonly used. Incubation should be performed at a temperature of 26-27°C and may require up to 4 weeks before a culture can be considered definitively negative.
-
Colony identification: Identification is based on a combination of criteria:
-
Macroscopic: Appearance of the colony (color, texture – cottony, powdery, granular), growth rate, and possible production of a pigment diffusing into the agar or visible on the reverse side of the colony.
-
Microscopic: After sampling a portion of the colony (often using transparent adhesive tape applied to the surface then transferred to a slide) and staining (classically with lactophenol blue), observation of macroconidia and microconidia (shape, size, wall, septation) is decisive for species identification. It is crucial to remember that macroconidia are structures produced in vitro (in culture) and are generally not observed on direct samples from the animal.
-
-
DTM (Dermatophyte Test Medium): This differential medium is a modified SDA with the addition of a pH indicator (phenol red) and inhibitory agents (such as cycloheximide to inhibit fast-growing saprophytes, and antibiotics like gentamicin and chlortetracycline to inhibit bacteria). The principle is based on the preferential metabolism of dermatophytes: they first use the protein sources in the medium, producing alkaline metabolites that turn the pH indicator from yellow to red. Saprophytic fungi, on the other hand, tend to use carbohydrates first (acidification, therefore no initial color change or a change to yellow), then, if the culture is prolonged, can also metabolize proteins, leading to a late red color change that can be confusing.
-
DTM interpretation: An early red color change, appearing at the same time as or before visible colony growth (usually within 3 to 7 days), associated with a compatible colony appearance (often white, cream, fluffy or powdery), is strongly suggestive of a dermatophyte.
-
DTM limitations: Interpretation of DTM in general practice can be less reliable than in specialized mycology laboratories. An Israeli study showed only an 80% agreement rate between clinic and laboratory readings, with false positives and false negatives more frequent in clinics [17]. Factors such as too low an ambient incubation temperature can delay the color change. Moreover, prolonged incubation can lead to a red color change by saprophytic fungi, a source of diagnostic error.
-
4.4. Histopathology: When the Lesion is Deep or Atypical
Histopathological examination of skin biopsies can be particularly informative, especially for nodular forms or when other tests are inconclusive.
-
Visualization of fungal elements: Hyphae can be visualized in the hair shaft, in hair follicles, or sometimes freely in the dermis in case of furunculosis. Spores can also be observed around hairs. The use of special stains such as PAS (Periodic Acid-Schiff) or GMS (Grocott Methenamine Silver) is often essential to clearly highlight fungal structures, which can be discrete with standard H&E staining.
-
Associated inflammatory patterns:
-
In the case of M. persicolor, inflammation can be discrete, with mainly lymphocyte infiltration in the scales of the stratum corneum.
-
For most other invasive dermatophytes, folliculitis (inflammation of the hair follicle), perifolliculitis, or even furunculosis (rupture of the follicle with intense inflammatory reaction in the dermis) can be observed.
-
In cases of kerion or pseudomycetoma, deep inflammatory nodules are typically observed, often granulomatous or pyogranulomatous, containing fungal elements, sometimes in the form of “grains.”
-
4.5. PCR (Polymerase Chain Reaction): An Emerging Molecular Tool
PCR allows sensitive detection of fungal DNA from hair and scale samples.
-
Principles and targets: Veterinary PCR panels generally target conserved DNA sequences in dermatophytes, allowing group detection (for example, Microsporum spp., Trichophyton spp.). More specific primers can then be used to identify certain species of major interest, such as M. canis.
-
Interpretation and nuances:
-
A positive PCR in an animal with compatible clinical signs is strongly suggestive of an active infection.
-
In a clinically healthy animal, a positive PCR may indicate asymptomatic carriage or mere transient environmental contamination of hair. The detection threshold for PCR is often very low.
-
A major limitation of PCR is its ability to detect fungal DNA whether it comes from viable or non-viable organisms. Thus, PCR can remain positive for some time after effective antifungal treatment, simply by detecting DNA from dead spores. It therefore does not necessarily confirm an active ongoing infection and its usefulness for therapeutic monitoring is debated.
-
-
Comparison with fungal culture: According to mycology expert Patrick Bourdeau, fungal culture, when performed and interpreted by a specialized laboratory, may prove more sensitive than some commercial PCR tests. Furthermore, culture offers the crucial advantage of enabling precise species identification (essential for epidemiology and research into the source of contamination) and confirming the viability of the fungus.
-
Consensus recommendations: The 2017 consensus on feline dermatophytosis from the International Society of Companion Animal Infectious Diseases (ISCAID) recognizes PCR as a useful diagnostic tool but emphasizes that its interpretation must be cautious and contextualized with clinical and epidemiological data [18].
4.6. Fluorescence Microscopy with Calcofluor White: Improving Direct Detection
Calcofluor White is a non-specific dye that binds with high affinity to cellulose and chitin, major components of fungal cell walls.
-
Technique: Hair and scale samples are first treated with a KOH solution (to clarify host cellular debris), then a drop of Calcofluor White is added. After a short incubation time, the sample is examined under a microscope equipped with a UV light source and appropriate filters (usually for excitation in near UV and emission in blue or green).
-
Advantages: Fungal elements (hyphae, spores) then appear brightly fluorescent, standing out clearly from the non-fluorescent background. This technique significantly increases the sensitivity and speed of direct microscopic detection compared to conventional white light examination. It has been reported that the use of Calcofluor White can practically double the sensitivity of direct microscopy.
Dermatophytosis is a true crossroads of diagnostic challenges. How does one find one’s way?
-
The great clinical variability: It requires always including dermatophytosis in the differential diagnosis of numerous skin conditions, even those that do not present the “classic” appearance.
-
The absence of a single, infallible “gold standard”: Recent expert consensuses emphasize that no diagnostic test, taken in isolation, is perfect [18]. A combined approach is often the most fruitful. The combination of Wood’s lamp examination (if M. canis infection is suspected) and direct microscopic examination (ideally with Calcofluor White to increase its sensitivity) constitutes an excellent first line of investigation in the clinic.
-
The environmental persistence of spores: M. canis spores can remain viable in the environment for periods of up to 14 months or more. This longevity significantly complicates infection management, particularly the prevention of reinfections and transmission to other animals or humans. Clipping infected animals (if feasible and well tolerated) can help reduce the environmental load of contaminated hair and thus spores.
-
The constant zoonotic risk: The infectivity of the animal to humans decreases with the institution of effective antifungal treatment, but precautionary measures (strict hygiene, limitation of close contacts, especially for children, the elderly, or immunocompromised individuals) must be maintained throughout the treatment and until mycological cure is confirmed.
-
Deep nodular forms (kerion or pseudomycetoma): Their diagnosis can be particularly arduous and often delayed if the initial suspicion of dermatophytosis is low. In these cases, histopathological examination of deep biopsies, with special stains for fungi, and fungal culture from the biopsied tissue are frequently indispensable.
-
Critical interpretation of test results and their intrinsic limitations:
-
Direct microscopy: Its sensitivity is highly dependent on the operator’s experience and the rigor of the technique employed (particularly adequate condenser adjustment).
-
DTM in practice: The risk of misinterpreting the color change (confusion with the growth of saprophytic fungi in case of late reading or prolonged incubation) is a recognized limitation.
-
PCR: Although very sensitive, PCR does not distinguish DNA from an active infection from the mere presence of viable or non-viable spores. Therefore, a positive PCR on an animal undergoing treatment or recently treated does not necessarily indicate therapeutic failure.
-
Fungal culture: Considered a reference method for species identification and confirmation of pathogen viability, culture may nevertheless be falsely negative if the sample is inadequate, if topical antifungals have been recently applied to the lesions, or if the laboratory technique is not optimal. It can also be contaminated by fast-growing saprophytic fungi that can mask or be confused with dermatophytes.
-
-
The impact of inappropriate corticosteroid use: Administration of glucocorticoids, whether by systemic or topical route, in the absence of a precise etiological diagnosis, can significantly worsen pre-existing dermatophytosis (incognito dermatophytosis) or mask its clinical signs, making subsequent diagnosis more complex and treatment longer.
-
The concept of infectious dose and immunity: A certain quantity of fungal spores is necessary to initiate a clinical infection. Animals that develop an effective immune response following a first infection may exhibit increased resistance to a subsequent reinfection by a similar dose of spores.
6. Conclusion and Perspectives: Towards an Enlightened Practice
Dermatophytosis, by its protean nature and the inherent challenges to its diagnosis, requires constant vigilance and a strategic diagnostic approach from the veterinary clinician. There is no infallible shortcut. Recognition of the various clinical manifestations, understanding the limitations and advantages of each diagnostic tool, and integration of epidemiological data are the pillars of a successful approach.
The future probably lies in the optimization and intelligent combination of existing techniques. Direct microscopy, enhanced by tools like Calcofluor White, retains a place of choice for rapid diagnosis in the clinic. Fungal culture, ideally performed in specialized laboratories, remains essential for precise identification and to evaluate viability, especially in complex cases or for therapeutic monitoring. PCR, meanwhile, offers high sensitivity but its interpretation must be cautious and always correlated with the clinical context.
Perhaps we will witness the emergence of rapid “point-of-care” molecular tests that will combine sensitivity and specificity while informing on viability? Or more standardized diagnostic algorithms integrating the strengths of each method?
While awaiting these advances, the key message remains: a high clinical suspicion, judicious selection of tests based on the case, and critical interpretation of results are the guarantors of optimal management of this fungal condition, for the well-being of our patients and the peace of mind of their owners.
References
[1] Weitzman I, Summerbell RC. The dermatophytes. Clin Microbiol Rev. 1995 Apr;8(2):240-59.
[2] de Hoog GS, Guarro J, Gené J, Figueras MJ. Atlas of Clinical Fungi. 4th ed. Centraalbureau voor Schimmelcultures; 2020.
[3] Moriello KA, Coyner K, Paterson S, Mignon B. Diagnosis and treatment of dermatophytosis in dogs and cats. Clinical Consensus Guidelines of the World Association for Veterinary Dermatology. Vet Dermatol. 2017 Jun;28(3):266-e68.
[4] Kano R, Hirai A, Yoshioka N, et al. Arthroderma vanbreuseghemii/Trichophyton mentagrophytes complex isolated from an Australian Cavy. Med Mycol J. 2009;50(3):309-12.
[5] Sparkes AH, Robinson A, MacKay AD, et al. A study of the dermatophytes of dogs and cats in the south of England. J Small Anim Pract. 1993 Oct;34(10):507-13.
[6] Donnely T. Personal communication/unpublished data cited in the presentation. (Note: This would require a formal citation if available, or acknowledgement of the source.)
[7] Miller WH Jr, Scott DW, Wellington JR. Isolation of dermatophytes from the haircoats of normal dogs and cats in the southeastern United States. J Am Anim Hosp Assoc. 1991;27:555-8.
[8] Kaplan W, Georg LK, Ajello L. Recent developments in animal ringworm and their public health implications. Ann N Y Acad Sci. 1958;70:636-49.
[9] Bourdeau P. Dermatophyties des carnivores domestiques : aspects épidémiocliniques et diagnostiques. Point Vét. 2005;36(254):44-51.
[10] Schaer M. Clinical Medicine of the Dog and Cat. 2nd ed. Manson Publishing; 2010. (Note: Attributing this specific quote directly to a publication by Schaer would require verification if not explicitly stated as such in the audio.)
[11] Scott DW, Miller WH Jr, Griffin CE. Muller and Kirk’s Small Animal Dermatology. 7th ed. Elsevier Health Sciences; 2012.
[12] Dekeyser H, Adriaensen C, Mignon B, et al. Asymptomatic carriage of dermatophytes by dogs and cats. Vet Dermatol. 2009 Aug;20(4):253-8.
[13] Čonková E, Kollarova L. Dermatophytes isolated from asymptomatic guinea pigs and rabbits in Slovakia. Mycoses. 2010 Jul;53(4):325-8.
[14] Kraemer A, Mueller RS, Schauer U, et al. Dermatophytes in pet guinea pigs and rabbits. Vet Microbiol. 2012 May 25;157(1-2):208-13.
[15] Cafarchia C, Figueredo LA, Otranto D. Fungal diseases of rabbits. Vet Microbiol. 2013 Nov 15;167(1-2):227-43.
[16] Newbury S. Wood’s lamp examination in small animal practice. Vet Clin North Am Small Anim Pract. 2000 Nov;30(6):1099-105.
[17] Kuzi S, Nivy R, Lavy E, et al. Comparison of real-time PCR and dermatophyte test medium culture for the diagnosis of dermatophytosis in a referral hospital setting. Vet Dermatol. 2016 Feb;27(1):32-e9.
[18] Moriello KA, Coyner K, Paterson S, Mignon B. Diagnosis and treatment of dermatophytosis in dogs and cats. Clinical Consensus Guidelines of the World Association for Veterinary Dermatology. Vet Dermatol. 2017 Jun;28(3):266-e68.
Search terms
diagnosis and treatment of dermatophytosis in dogs and cats, topical therapy, infected animals, veterinary dermatology, clinical consensus guidelines, feline leukemia virus, veterinary medicine, fungal culture, skin lesions, systemic therapy, dogs and cats, j feline med surg, infected cats, infected hairs, fungal dna, topical treatment, active infection, persian cats, clinical cure, canine and feline dermatophytosis, clinical signs, feline med surg, experimental microsporum canis infection, environmental contamination, world association, systemic antifungal drugs, lime sulfur, hair coat, cats infected, skin disease, fungal spores, microsporum canis infection, canis infection, mycological cure, systemic treatment, fungal organisms, hair follicles, underlying disease, hair shafts, allergic dermatitis, vet dermatol, fungal vaccines, world association for veterinary, association for veterinary dermatology, concurrent lime sulphur rinses, improved molecular diagnostic assay, wood’s lamp examination, feline dermatophytosis, disease identification, cats diagnosed, kill spores, risk factors, accelerated hydrogen peroxide, dermatophyte test medium, compounded formulations, effective treatment, mineral oil, normal cats, wood’s lamp, treat dermatophytosis, nodular lesions, infective spores, cats clinical consensus guidelines, antifungal agents, adverse effects, false negative results, microscopic examination, chemical reaction, other pets, reduce environmental contamination, northwestern us animal shelter, pulse therapy, itraconazole oral solution, steam cleaning, small animals